Is eczema more than just an itchy rash? Exploring the depths of this common skin condition could unlock lasting relief. Let’s dive into the symptoms, causes, and treatment options for managing this frustrating skin issue.
Key Takeaways
- Eczema, or atopic dermatitis, is a chronic skin condition that affects over 31 million Americans.
- Symptoms can include dry, itchy, red, and inflamed skin that may worsen due to triggers like irritants or allergens.
- Eczema often starts in childhood but can persist into adulthood, with periods of flare-ups and remission.
- Understanding the underlying causes, risk factors, and effective management strategies is key to managing eczema.
- Proper skin care, identifying and avoiding triggers, and exploring treatment options can help control eczema symptoms and improve quality of life.
What is Eczema and Its Impact on Daily Life
Eczema, also known as atopic dermatitis, is a chronic skin condition causing inflammation and irritation. It affects over 31.6 million people in the U.S., or 10.1% of the population. Early childhood is when eczema peaks, with 1 in 10 individuals developing it at some point.
Different Names for Eczema
While “eczema” is widely used, the medical field also calls it “atopic dermatitis.” These terms are often used interchangeably to describe the same condition.
Statistics and Prevalence
Eczema significantly impacts a person’s quality of life. In the U.S., about 9.6 million children under 18 have atopic dermatitis, with a third experiencing severe symptoms. The prevalence of childhood eczema has risen from 8% to 15% between 1997 and now. Among adults, 16.5 million have it, with nearly 40% facing moderate to severe symptoms.
How Eczema Affects Quality of Life
The constant itching, skin redness, and sleep disturbances from eczema are overwhelming. Over 60% of adults with moderate to severe atopic dermatitis experience severe or unbearable itch, and more than half report inadequate disease control. Eczema also causes emotional distress, social challenges, and can even shorten lifespan due to hospitalizations during flare-ups.
“Itch, skin redness, and sleep loss are the most burdensome symptoms of AD.”
Common Symptoms and Signs Across Different Skin Types
Eczema symptoms vary greatly depending on an individual’s skin tone. In those with lighter skin, eczema rashes often show as red, pink, or purple. In contrast, darker skin may display rashes as purple, brown, or gray.
Across all skin colors, eczema symptoms include intense itchy skin, dry and cracked skin, swelling, and a thickened or leathery texture. Infants often see eczema on their face and scalp. Children and adults, on the other hand, experience it more on the bends of elbows, back of knees, neck, wrists, and ankles.
As eczema progresses, the skin can become thick, scaly, and discolored. Flare-ups can occur for years, affecting various body parts. Common skin infections such as staph, molluscum contagiosum, and eczema herpeticum also plague those with eczema.
Research indicates that eczema’s presentation changes with age and race. This affects both symptom severity and the body areas affected. Grasping these differences is key to diagnosing and managing this chronic condition effectively.

| Skin Tone | Common Eczema Symptoms |
|---|---|
| Lighter Skin | Red, pink, or purple rashes |
| Darker Skin | Purple, brown, or gray discoloration |
| All Skin Tones | Extreme itchiness, dry and cracked skin, swelling, thickened or leathery texture |
“Eczema affects 31 million people in the United States, and the presentation can vary significantly based on an individual’s age and race.”
Types of Eczema and Their Characteristics
Eczema encompasses several distinct skin conditions, each with its own set of symptoms and triggers. Understanding these different types is key to managing this chronic condition. Let’s dive into the most common forms of eczema and their unique features.
Atopic Dermatitis
Atopic dermatitis, the most common form of eczema, often starts in childhood. It’s linked to other allergies like asthma and hay fever. The skin becomes dry, itchy, and inflamed, potentially thickening and changing color over time.
Contact Dermatitis
Contact dermatitis happens when the skin reacts to an irritant or allergen. This results in a red, itchy rash. It can be caused by harsh chemicals (irritant contact dermatitis) or an immune reaction to a specific allergen (allergic contact dermatitis).
Other Common Types
- Dyshidrotic Eczema: This type affects the hands and feet, causing small, fluid-filled blisters that can be incredibly itchy.
- Neurodermatitis: Also known as lichen simplex chronicus, neurodermatitis leads to thick, scaly, and intensely itchy patches on various parts of the body, often due to chronic rubbing or scratching.
- Nummular Eczema: Characterized by round, coin-shaped spots that can be itchy and persist for several years, nummular eczema is sometimes triggered by a skin injury.
- Seborrheic Dermatitis: This type mainly affects the scalp, causing oily, flaky, and sometimes itchy patches, and may also appear on other oil-rich areas of the body.
- Stasis Dermatitis: Occurring in individuals with poor circulation, typically in the lower legs, stasis dermatitis can cause swelling, skin discoloration, and itchy rashes.
Each type of eczema has its own set of symptoms, triggers, and management strategies. This highlights the importance of working closely with a healthcare professional to develop a personalized treatment plan.
| Eczema Type | Key Characteristics | Prevalence |
|---|---|---|
| Atopic Dermatitis | Dry, itchy, and inflamed skin; often begins in childhood | Affects over 7% of American adults |
| Contact Dermatitis | Red, itchy rash caused by exposure to irritants or allergens | Nearly everyone experiences it at some point |
| Dyshidrotic Eczema | Small, fluid-filled blisters on hands and feet | Less common type of eczema |
| Neurodermatitis | Thick, scaly, and intensely itchy patches | More common in individuals assigned female at birth between ages 30-50 |
| Nummular Eczema | Round, coin-shaped spots that can be itchy and persistent | May be triggered by a skin injury and linked to allergies or asthma |
| Seborrheic Dermatitis | Oily, flaky, and sometimes itchy patches on the scalp and other oil-rich areas | Known as dandruff when affecting the scalp |
| Stasis Dermatitis | Swelling, skin discoloration, and itchy rashes in the lower legs due to poor circulation | More common in individuals with vein problems in their legs |
Recognizing the unique characteristics of each eczema type is the first step toward effective management and relief from this chronic skin condition.
Understanding the Root Causes of Eczema
The exact causes of eczema are not fully understood. Yet, research indicates that both genetic and environmental factors are key. These elements play a significant role in the development and progression of this skin condition. Let’s explore the underlying causes of eczema.
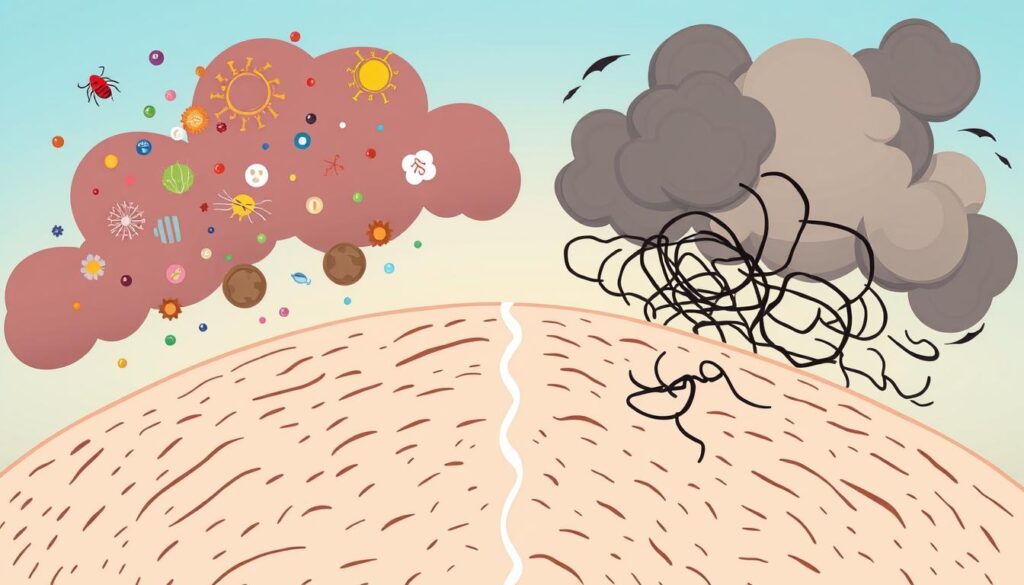
An overactive immune system is a primary contributor to eczema. People with eczema often have an exaggerated immune response to certain triggers. This leads to inflammation and skin irritation. Genetic factors are believed to influence this heightened immune activity, making some more susceptible to eczema.
The skin barrier function is another critical factor. Healthy skin acts as a protective barrier, keeping us safe from external irritants and maintaining moisture. In eczema, this barrier is compromised. This allows allergens and irritants to penetrate more easily, triggering flare-ups.
Genetic factors also significantly contribute to eczema. Studies have shown that those with a family history of eczema are more likely to develop it. Certain gene variations can affect the skin’s protective mechanisms, increasing susceptibility to this skin disorder.
Environmental triggers, such as certain chemicals, fragrances, and stress, also play a role. These factors can interact with the immune system and skin barrier, worsening eczema symptoms.
Understanding the complex interplay of these root causes is essential. It helps us better manage and treat eczema. This offers hope to those affected by this challenging skin condition.
“Eczema is a complex condition that involves multiple factors, including the immune system, skin barrier, and genetics. By addressing these underlying causes, we can better support those living with eczema.”
| Factor | Contribution to Eczema |
|---|---|
| Immune System | Overactive immune response leading to inflammation |
| Skin Barrier | Compromised barrier allowing irritants to penetrate |
| Genetics | Genetic variations affecting skin protection and susceptibility |
| Environmental Triggers | Chemicals, fragrances, and stress exacerbating symptoms |
Risk Factors and Genetic Predisposition
Eczema, a chronic skin condition, is influenced by various risk factors. These include age, environmental triggers, and genetic predisposition. Understanding these elements is key to managing and preventing eczema.
Age-Related Risk Factors
Eczema often appears early in life, with about 70% of cases showing up before age 5. It typically starts in childhood, with severity potentially decreasing over time. Yet, adult-onset eczema is common, affecting around 1 in 10 adults.
Environmental Influences
Environmental factors significantly impact eczema development. Exposure to harsh chemicals, pollution, or extreme weather can trigger flare-ups. Living near factories, major roadways, or wildfire-affected areas also raises eczema risk.
Family History Considerations
Genetic predisposition is a major risk factor for eczema. Those with a family history of allergies or asthma are more likely to develop eczema. Studies indicate a 75% chance of inheriting eczema. Certain genetic variations, like FLG gene mutations, significantly increase this risk.
In summary, eczema risk factors include age, environmental triggers, and genetic predisposition. By understanding these factors, individuals can proactively manage their skin health and lessen eczema’s impact on their lives.
“Understanding the underlying causes and risk factors of eczema is the first step in effectively managing the condition and preventing flare-ups.”
Identifying Common Triggers and Irritants
Managing eczema, a chronic skin condition, often involves pinpointing and avoiding personal triggers. While the root causes of eczema are complex, understanding common triggers and irritants can help individuals with eczema take proactive steps to prevent flare-ups and maintain healthier skin.
Eczema triggers can vary widely from person to person, but some of the most frequent culprits include stress, temperature changes, sweating, certain fabrics like wool, harsh soaps or detergents, dust mites, pet dander, pollen, mold, and specific foods like dairy, eggs, and nuts.
- Environmental factors, such as low humidity, cold weather, or hot and humid conditions, can also exacerbate eczema symptoms.
- Irritants like chemicals, fragrances, and preservatives found in personal care products can disrupt the skin’s protective barrier, leading to flare-ups.
- Genetic factors and family history also play a significant role in determining individual eczema triggers.
Identifying and avoiding personal eczema triggers is key to managing the condition. By keeping a detailed diary of symptoms, tracking triggers, and working with healthcare professionals, individuals can develop strategies to minimize flare-ups. This helps maintain healthier, more comfortable skin.
“Eczema is often known as atopic dermatitis and is caused by a complex interaction between a person’s environment and their genes, leading to an overactive immune system response to irritants or allergens.”
Stress management, maintaining a consistent skincare routine, and addressing any underlying allergies or sensitivities can all contribute to better eczema control. By understanding and proactively managing eczema triggers, individuals with this chronic condition can improve their quality of life and find relief from disruptive symptoms.
Hives vs Eczema: Understanding the Differences
Hives and eczema both cause itchy skin, but they look and last differently. Hives are raised, red welts that move around and usually go away in a few days. Eczema, by contrast, is dry and scaly, lasting longer.
Appearance and Duration
Hives are a quick allergic reaction to things like food, medicine, or the environment. They come and go fast, lasting hours or days. Eczema, a chronic condition, can flare up and settle down over time. Its dry, inflamed patches can last weeks or months.
Treatment Approaches
- Hives are often treated with over-the-counter antihistamines to reduce itching and swelling.
- Eczema treatment involves moisturizing and controlling inflammation, often with prescription creams.
- Staying away from triggers is key for both hives and eczema to prevent outbreaks.
Knowing the differences between hives and eczema helps manage skin allergies better. Recognizing their unique traits allows us to make informed choices about our skin health. This way, we can find relief more effectively.
Treatment Options and Management Strategies
Effective eczema treatment aims to relieve symptoms and prevent flare-ups. A combination of strategies is often necessary, including regular moisturizing, gentle skincare products, and avoiding triggers. Let’s explore the various treatment options available to manage eczema effectively.
Topical Treatments
Over-the-counter (OTC) topical treatments can provide temporary relief for eczema symptoms. Topical hydrocortisone, a low-potency steroid, can soothe itching and redness. Medicated shampoos containing ingredients like ketoconazole, selenium sulfide, coal tar, and zinc pyrithione can address scalp-related eczema.
Prescription-strength topical treatments include corticosteroids, calcineurin inhibitors, PDE4 inhibitors, and Janus kinase (JAK) inhibitors. These targeted therapies reduce inflammation and regulate the immune response. They offer more long-term relief for moderate to severe eczema.
Systemic Treatments
In severe or persistent cases, healthcare providers may recommend systemic treatments. Oral antihistamines can alleviate itching. A diluted bleach bath can help reduce bacterial infections on the skin.
For patients with moderate to severe atopic dermatitis, injectable biologics like dupilumab (Dupixent) and tralokinumab (Adbry) may be prescribed. They target the underlying immune system dysfunction.
Skincare Routine
Maintaining a consistent and gentle skincare routine is essential for managing eczema. This includes daily bathing, immediate moisturizing, and avoiding harsh soaps and irritants. Keeping the skin hydrated and protected can prevent flare-ups and reduce symptoms’ severity.
| Treatment Type | Examples | Targeted Symptoms |
|---|---|---|
| Topical OTC | Hydrocortisone, medicated shampoos | Itching, redness, irritation |
| Prescription Topical | Corticosteroids, calcineurin inhibitors, PDE4 inhibitors, JAK inhibitors | Inflammation, immune regulation |
| Systemic | Oral medications, light therapy, biologics | Severe or persistent eczema, underlying immune dysfunction |
| Skincare Routine | Daily bathing, moisturizing, gentle products | Hydration, prevention of flare-ups |
By working closely with healthcare professionals, individuals with eczema can develop a tailored treatment plan. This plan combines various approaches to effectively manage their condition and improve their quality of life.
Best Eye Cream for Eczema on Eyelids
Choosing the right eye cream is vital for eczema-prone eyelids. It must be gentle, fragrance-free, and packed with ingredients that soothe and repair. Look for ceramides, hyaluronic acid, and niacinamide. These strengthen the skin’s barrier, reduce inflammation, and hydrate.
Recommended Ingredients
Opt for eye creams tailored for sensitive, eczema-prone skin. Ceramides, hyaluronic acid, and niacinamide are key. They restore the skin’s barrier, retain moisture, and lessen redness and irritation. Steer clear of harsh chemicals, alcohols, and fragrances, as they can irritate the delicate eye area.
Application Tips and Safety
Apply eye cream for eczema with care, avoiding tugging or pulling. Dab it around the orbital bone, but avoid the eyes. Always test a small area first to prevent irritation. If eczema worsens or doesn’t respond to over-the-counter treatments, see a dermatologist. They may suggest a medicated cream or ointment for the eyes.
FAQ
What is eczema and how common is it?
Eczema is a non-contagious skin condition causing dry, itchy patches. It affects over 31 million Americans. Symptoms include red, dry, cracked, swollen, or thickened skin. It often starts before age 5 and can continue into adulthood.
How does eczema impact daily life?
Eczema, or atopic dermatitis, can significantly affect quality of life. It causes sleep problems, emotional distress, and social challenges. Over 7% of American adults suffer from it.
How do eczema symptoms differ across skin tones?
In lighter skin, eczema rashes appear red, pink, or purple. In darker skin, they can be purple, brown, or gray. Symptoms include extreme itchiness, dry and cracked skin, swelling, and thickened skin.
What are the different types of eczema?
There are several types, including atopic dermatitis (most common), contact dermatitis, dyshidrotic eczema, and others. Each type has unique characteristics and triggers.
What causes eczema?
The exact cause is unknown, but it involves genetic and environmental factors. It may be related to an overactive immune response or skin barrier problems.
What are the risk factors for developing eczema?
Risk factors include family history of allergies or asthma, very dry skin, and exposure to pollution. Age and genetic predisposition also play a role.
What are common eczema triggers?
Common triggers include stress, temperature changes, sweating, and certain fabrics. Harsh soaps, dust mites, pet dander, pollen, and mold can also trigger flare-ups.
How do hives and eczema differ?
Hives and eczema both cause itchy skin but differ in appearance and duration. Hives are raised, red welts that resolve within hours or days. Eczema is dry, scaly patches that last longer. Hives are often an allergic reaction, while eczema is chronic.
What are the treatment options for eczema?
Treatment aims to relieve symptoms and prevent flare-ups. Strategies include moisturizing, using gentle skincare, and avoiding triggers. Topical treatments include corticosteroid creams and calcineurin inhibitors. For severe cases, oral medications or light therapy might be prescribed.
What should I look for in an eye cream for eczema on eyelids?
Look for gentle, fragrance-free products with ceramides, hyaluronic acid, and niacinamide. Avoid harsh chemicals and irritants. Always patch test and apply gently. For severe cases, consult a dermatologist for specific recommendations.

